- Research
- /
- The relationship between epilepsy and Alzheimer's dementia
The relationship between epilepsy and Alzheimer's dementia
Supporter
National Brain Research Programme I (KTIA_NAP_13-1-2013-0001
Research leader
Prof. Dr. Anita Kamondi
Duration
2013-2017
Témafelvetés:
Alzheimer's Disease (AD) is one of the greatest medical challenges of the developed world, crippling hundreds of millions of lives worldwide, and we must act in every way we can to cure and prevent this disease. The brain structure most affected by AD is a part of the temporal lobe, the hippocampus, which is also one of the most epileptogenic areas of our brain. Over the past two decades, several animal studies have shown that epileptic seizures are more frequent in AD and are a feature of the disease, contributing significantly to the development of its symptoms and facilitating its more rapid progression. Their treatment with medication improved the condition and survival of animals. In humans, the actual frequency of seizures, and thus the effect of anti-epileptic drug therapy, has not yet been elucidated, as it is assumed that epilepsy occurs in the deep layers of the brain, which cannot be accessed by simple or short-term studies.
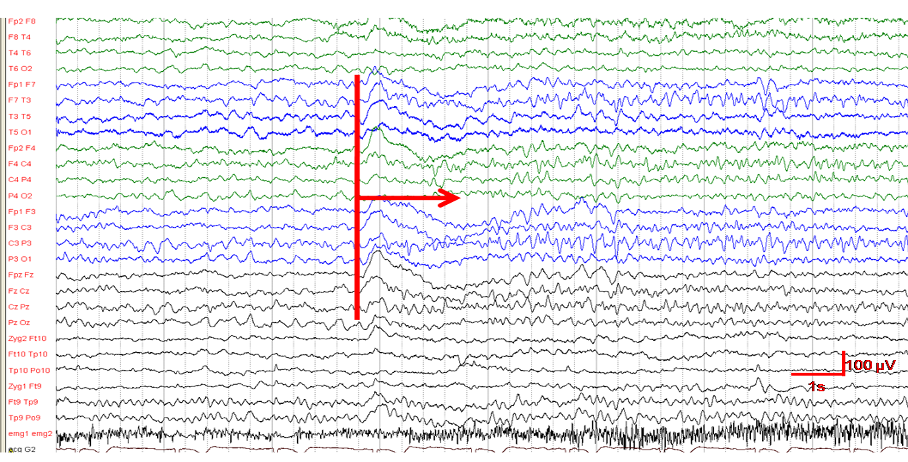
We hypothesised that in patients with Alzheimer's disease, epileptic activity from the temporal lobe may be more intense than previously estimated. This also raised the possibility that complex partial seizures may underlie the transient and fluctuating memory and behavioural changes seen in the disease. Our group has shown that long-term electroencephalography (EEG) and video EEG monitoring in conjunction with sleep studies are more suitable for detecting this type of epileptiform activity than routine scalp EEG studies. Thus, the overall aim of our study was to estimate and analyse epileptiform activity in a population of patients with mild to moderate Alzheimer's disease (AD) using long-term and video EEG monitoring. We believed that as a result, EEG findings could become a potential biomarker of AD and, with follow-up studies, possibly a prognostic factor for the changes seen in EEG. It is also conceivable that antiepileptic therapy could have a positive impact on the symptoms and course of the disease in selected cases.
Eredmények:
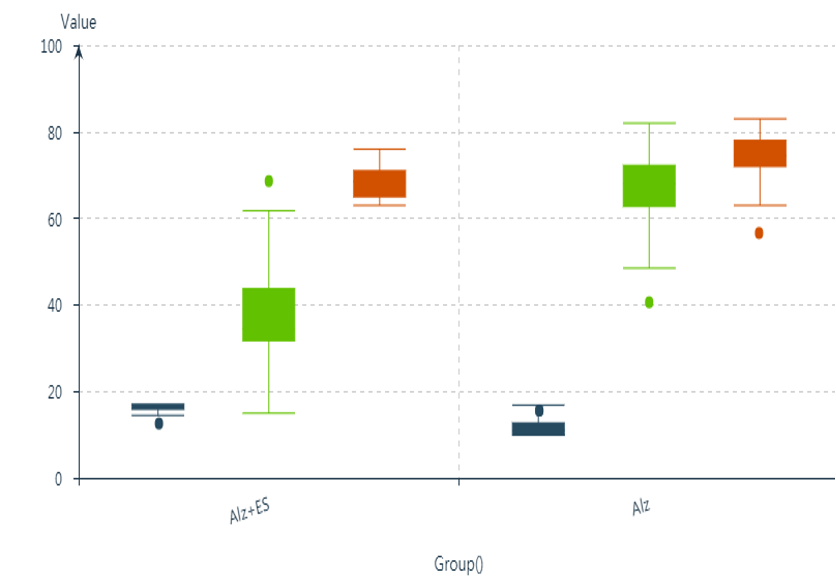
Our studies were conducted between 2013 and 2017, during which we performed 24-hour Holter-EEG scans of 70 patients with dementia previously diagnosed with Alzheimer's disease (AD), and evaluated the results from an epileptological perspective. We were able to confirm the diagnosis of AD in 55 patients by reviewing clinical data, neuropsychological and imaging findings. A clinically important observation was that 21% of the patients did not meet the diagnostic criteria for AD, and in many cases a reversible form of dementia was identified. Twenty-one patients were followed neuropsychologically for 2 years and sleep parameters of 30 AD patients were compared with a sample of healthy individuals. We found that a quarter of patients had detectable epileptic seizures, mainly occurring in patients with dementia that started at an early age, had a longer duration and a more severe stage. The seizures are mainly complex-partial seizures with temporal lobe origin without movement symptoms. Epileptiform activity (EA) was recorded in half of the patients, often without epileptic seizures. EA occurred mainly in the frontotemporal areas (85%), with a strong left-sided predominance (65%), mainly during periods of slow-wave sleep (45%). During sleep assessment, we demonstrated that slow-wave sleep is significantly reduced in AD, the normal sleep structure is disrupted, and that REM sleep parameters may be important markers of disease progression. We further confirmed that 24-h Holter-EEG testing can be performed safely, easily and with high sensitivity in the detection of AD-related epilepsy. Our results highlighted the strong association between AD, sleep and epilepsy.

Last updated: 06.06.2021.